-28/11/17-

-28/11/17-
Had cramps so spent the day writing up microbiology notes whilst hunched over my hot water bottle. The lecture on vaccine design is 7 pages long and now I can hand cramp to my list of ailments…
More Posts from T-b-a-blr-blog and Others
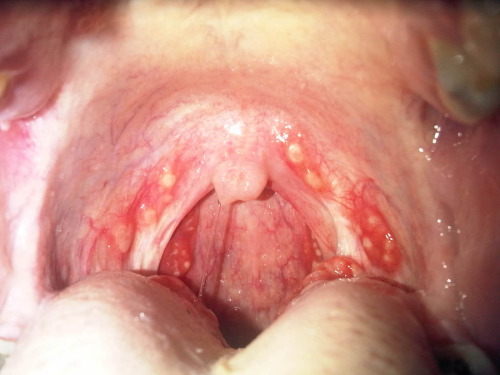
Strep throat.
Influenza
Happy flu season! I’ve just been stuck inside for 5 days with a mild case, so this is a bit bitter
There are 3–5 million cases of flu per year, and ~375,000 deaths, usually in older, younger, and immunocompromised individuals.
Enveloped, Single-stranded RNA virus
First identified in 1933, but existed long before
Generally considered an infection of the bronchi
so effectively a form of bronchitis – i.e. it causes inflammation of the bronchi
There are 3 types - A, B and C
B & C appear restricted to humans
C is less common
A is found in wide range of species including pigs and poultry as well as man
Type A appears to be responsible for more severe disease

Basics
Transmission by aerosols
Incubation ~2 days
Contagious during first 3-5days of illness
Symptoms – fever, myalgia, headache, dry cough, sore throat, aches, fatigue
Recovery ~7-10 days for most
Complications – most frequent = secondary bacterial pneumonia, rarely = viral pneumonia, myocarditis, encephalitis
No specific treatment
Vaccination for high risk groups including the elderly, health care workers, those with underlying respiratory conditions.
Avian
The main reservoir is wildfowl that are resistant to the disease
doesn’t usually affect animals other than poultry and pigs
However some transfer events occur
Seasonal
Incidence highest in winter
Strains vary from year to year - hard to predict and vaccinate (this year’s vaccine has been pretty rubbish)
Pandemic
Can be caused by any strain that has not been seen in the human population for many years
New strains evade the herd immunity that exists to previously encountered strains
1918 /19 –( Spanish) estimated 40-50 million deaths worldwide
1957 – Influenza A/H1N1 (Asian)
1968 – Influenza A/H3N2 (Hong Kong)
Eventually the virus runs out of susceptible hosts and the epidemic fizzles out
Experts generally agree another pandemic is inevitable, and may be imminent – maybe we have had some minor pandemics
16000 confirmed H1N1 deaths in 2009 affecting over 200 countries
Consensus is that the prompt action of the Hong Kong authorities probably prevented a pandemic in 1997
The prediction is scary - for industrialised countries they predic 1.0 – 2.3 million hospitalisations
280,000-650,000 deaths
in two years
A network of 112 centres monitor flu isolates to identify unusual strains that can then be examined further
The WHO has a Pandemic Preparedness Plan in place http://www.who.int/influenza/preparedness/pandemic/en/
Diagnosis
Generally based on GP diagnosis
Virus isolation / virus demonstration from nasopharyngeal secretions during acute phase
Demonstration of viral antigen in secretions
Antibody rise using paired sera ( 1st sample taken between days 1-3 of illness, 2nd taken around day 12 of illness) by haemagglutination inhibition or complement fixation test
Molecular methods evolving rapidly – in particular in response to the recent epidemic/pandemic strains emerging
A range of respiratory illnesses have the same symptoms, only laboratory testing can confirm the aetiological agent
Treatment/Vaccination
In the UK NICE argue that immunisation against predicted strains is the best form of defence – traditionally focused on the elderly and those with underlying lung problems, but recently started rolling out a childhood vaccine (nasal spray)
Vaccines generally based on the H & N surface structures which mutate, however hopes of an M protein based vaccine which will give longer lasting protection raised recently
Antivirals
Antivirals not recommended in otherwise healthy people (amantadine should not be used at all) - should ride it out
However when incidence reaches a certain level zanamivir and oseltamivir should be used in those considered high risk for the development of complications – PROVIDED THAT TREATMENT IS STARTED WITHIN 48 HOURS OF ONSET OF SYMPTOMS
Resistance is becoming an issue

PSEUDOmonas aeroginosa.
Pneumonia
Sepsis (black lesion on skin).
External otitis (swimmers ear)
UTI,Drug use .
Diabetic osteomylitis
Aminoglycoside„,extended spectrum penicillin(pipracilin,ticarcillin)
Think pseudomonas in burn victims

One possible cover design for The Book
Coming soon.
be patient, good things are coming your way :)

Diphtheria is known for creating a slimy/sticky/smelly exudate in the throat and mouth, but there are quite a few variations on its etiology and presentation.
A. Common type of diphtheria. Child three years old, seen on fourth day of illness. Exudate covering pharynx, tonsils, and uvula. Received 16,000 units of antitoxin. Throat clear on sixth day. Discharged cured.
B. Follicular type of diphtheria. Child seven years old, seen on second day of illness. The membrane involved the lacunae of the tonsils. Resembles follicular tonsillitis. Received 6,000 units of antitoxin total.
C. Hemorrhagic type of diphtheria. Child seven-and-a-half years old, seen on sixth day of illness. Tonsillar and post-pharyngeal exudate. Severe nasal and post-pharyngeal hemorrhages during exfoliation of membrane. Received in all 15,000 units of antitoxin. Throat clear on ninth day of illness. Myocarditis developed. Case discharged cured four weeks after admission.
D. Septic type of diphtheria. Child eight years old, seen on fifth day of illness. The pseudo-membrane in this case covered the hard palate and extended in one large mass down the pharynx, completely hiding the tonsils.
Diseases of Infancy and Childhood. Louis Fischer, M.D., 1917.

desmosome a circular, dense body that forms the site of attachment between certain epithelial cells, especially those of stratified epithelium of the epidermis, which consist of local differentiations of the apposing cell membranes.
-Exfoliatin
A staphylococcus toxin - Cleaves the desmosomes in the stratum granulosum - Separates layers of skin. - Example: Scalded skin syndrome (occurs more often in infants)

New background! Download higher quality photo here!
https://drive.google.com/file/d/1F5SlJmB8YiNNtGuKrc-QtMnrrjZ1tOHL/view?usp=sharing
Amazing web site!
Antimicrobial Agents - Inhibition of DNA and Protein Synthesis
Bacterial chromosome replication

DNA replication

Bacterial Topoisomerases
maintain DNA in appropriate state of supercoiling
cut and reseal DNA
DNA gyrase (topoisomerase II) introduces negative supercoils
Topoisomerase IV decatenates circular chromosomes
these are the targets of the quinolone antibacterial agents
Quinolones
bind to bacterial DNA gyrase and topoisomerase IV after DNA strand breakage
prevent resealing of DNA
disrupt DNA replication and repair
bactericidal (kill bacteria)
Fluoroquinolone is particularly useful against
Gram +ves: Staphylococcus aureus, streptococci
Gram -ves: Enterobacteriacea; Pseudomonas aeruginosa
Anaerobes: e.g. Bacteroides fragilis
many applications e.g. UTIs, prostatitis, gastroenteritis, STIs
Adverse effects
Relatively well tolerated
GI upset in ~ 5% of patients
allergic reactions (rash, photosensitivity) in 1 - 2% of patients

Inhibition of Bacterial Protein Synthesis
Macrolides
in 1952: Erythromycin was isolated as the first macrolide (Streptomyces erythreus)
Newer macrolides: clarithromycin, azithromycin
Structurally they consist of a lactone ring (14- to 16-membered) + two attached deoxy sugars
Mode of action
bind reversibly to bacterial 50S ribosomal subunit
causes growing peptide chain to dissociate from ribosome → inhibiting protein synthesis
bacteriostatic (stops reproduction)

Macrolides’ spectrum of activity
good antistaphylococcal and antistreptococcal activity
treatment of respiratory & soft tissue infections and sensitive intracellular pathogens • e.g. Chlamydia, Legionella
Adverse effects
Generally well tolerated
nausea
vomiting
diarrhoea
rash
Aminoglycosides
large family of antibiotics produced by various species of Streptomyces (“mycin”) and Micromonospora (“micin”)
include: streptomycin, neomycin, kanamycin, gentamicins, tobramycin
Structure = linked ring system composed of aminosugars and an aminosubstituted cyclic polyalcohol
Mode of action of aminoglycosides
Bind irreversibly to 30S ribosomal subunit
disrupt elongation of nascent peptide chain
translational inaccuracy → defective proteins
bactericidal

Spectrum of activity
broad spectrum; mainly aerobic G-ve bacilli (e.g. P. aeruginosa)
used to treat serious nosocomial infections (hospital acquired infections)
First TB antibiotic
Used for cystic fibrosis
Adverse effects
all aminoglycosides have low Therapeutic Index (only a small amount needed to become toxic)
renal damage, ototoxicity, loss of balance, nausea
-
 t-b-a-blr-blog reblogged this · 6 years ago
t-b-a-blr-blog reblogged this · 6 years ago -
 t-b-a-blr-blog liked this · 6 years ago
t-b-a-blr-blog liked this · 6 years ago -
 iladygodiva liked this · 7 years ago
iladygodiva liked this · 7 years ago -
 cellularstudy reblogged this · 7 years ago
cellularstudy reblogged this · 7 years ago -
 parchedspaghetti liked this · 7 years ago
parchedspaghetti liked this · 7 years ago -
 cellularstudy reblogged this · 7 years ago
cellularstudy reblogged this · 7 years ago